Before Brain Surgery
fMRI & PET Scan Report (2008/2009)
The tests showed my speech to be predominantly on the LEFT with very little speech on the right. My motor and sensory areas appeared to be a substantial distance away from the lesion. The good news was: There isn’t any language function within the lesion that is intended to be cut!
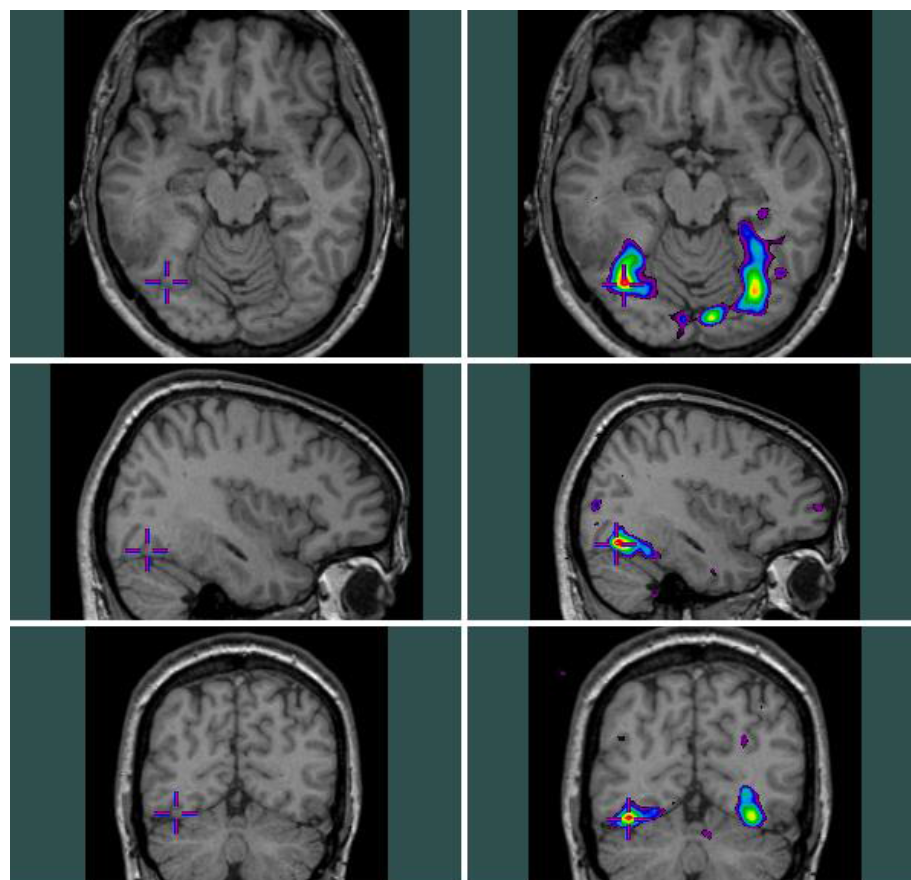
The above is part of the Imaging of Cognitive Functions using functional Magnetic Resonance Imaging (fMRI) can be downloaded here
PET Scan reports can be shared with you upon request. These tests allowed the surgeon to safely “cut” the brain areas needed. It is interesting to share that my brain function had moved over time (since childhood) away from where it would typically be, and that made it safe to undertake the surgery.
During Operation
The operation took around 11 hours. I was awake during the operation (on and off) for testing. The last time they woke me up resulted in me not being able to respond to questions properly (slower word finding, and sometimes not finding the word).
Therefore, they decided to stop the operation after cutting ~92% of the targeted tumor resection.
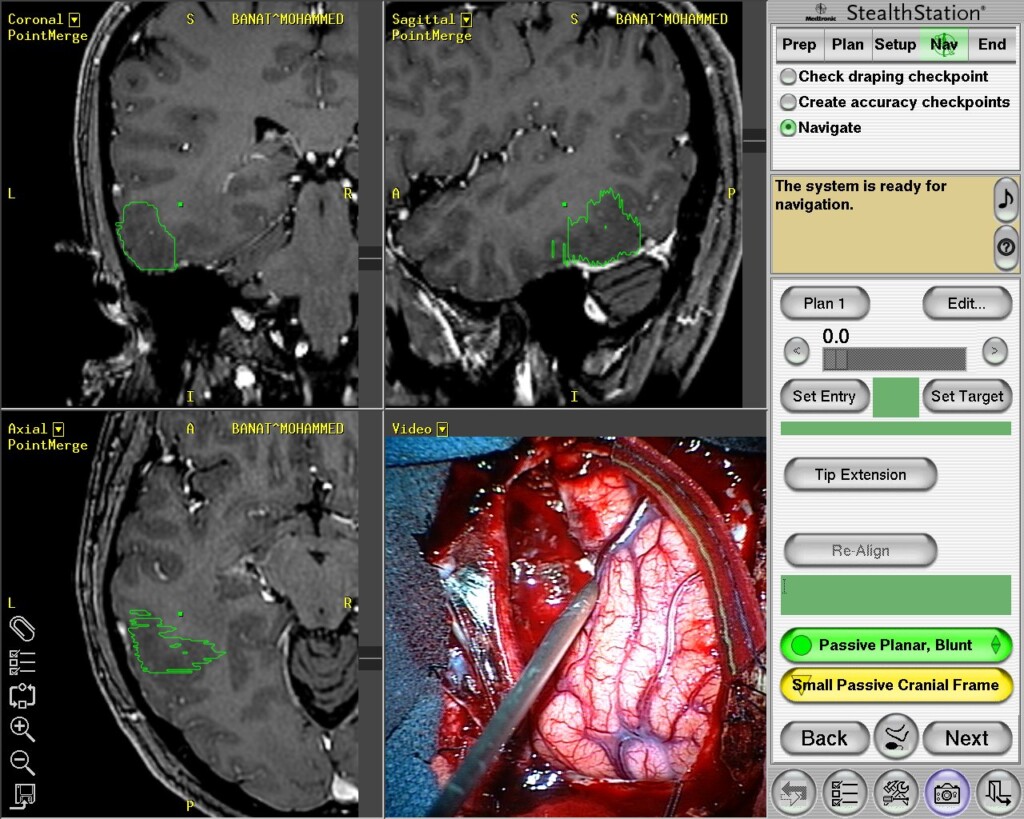
I have more photos of this sort, but they looked the same to me, so I decided to share only one at this stage. I can share the others upon request.
Right After Surgery
Post-surgery Report (2009)
The diagnostic was a low-grade astrocytoma (low-grade mixed glioma), WHO grade-II involving posterior left temporal lobe – MGMT promotor methylation.
There are three reports from the Montreal Neurological Institute and Hospital:
-
- Surgery and Operative Procedure (3 pages) Download here
-
- Post-Surgery Report (2 pages) Download here
-
- Addendum Report (3 pages) Downloaded here
Other Neuropathology Report (2009)
The most important facts are that my tumor is:
-
- Confirmed heterozygosity at 1p and 19q confirming an oligodendroglial component.
-
- Why is this important? Here’s a recent study from 2019 showing The Impact of MGMT Promoter Methylation and Temozolomide Treatment in Serbian Patients with Primary Glioblastoma. I did not take any action up until now, given that I am still in grade II.
I learned in 2016 that I should have checked for the IDH1 mutation with a test, but I did not do it yet, and I wasn’t sure if I should spend effort on that front.
Chemotherapy and Radiotherapy
Never done.
Second Opinion on Neuropathology
I sent a sample of the pathology from Canada to the United Kingdom. The purpose is for Cleveland to give me their second opinion.
Their work showed that what I gave is a low-grade oligoastrocytoma (low-grade mixed glioma), WHO grade II. That clearly is different from what Canada believed in.
The detailed report is very rich, and you can see many key pieces of information, including the prognosis.
In parts of their 19-page report, they said the following:
Mutations in isocitrate dehydrogenase 1 and 2 (IDH1 and IDH2) have been implicated in tumorigenesis of gliomas. Patients with high-grade astrocytomas with IDH1 or IDH2 mutations were reported to have a better survival. IDH1 mutations were present in the majority of progressive astrocytomas. No mutations in IDH2 were found. For low grade gliomas, presence of IDH1 mutations were early events and significantly improved overall survival (median survival 48 vs. 98 months).
These results indicate that IDH1 mutations identify a subgroup of gliomas with an improved survival. Dubbink et al, Neurology Nov 24;73 1792-5, 2009
A more recent review from Germany by Ahmadi et al J Neurooncology 2012 April (Epub ahead of print) looked at 100 low grade astrocytoma patients and found no difference in overall survival or progression free survival relative to IDH1 mutation state in patients who did not receive adjuvant treatment.While the IDH1 mutational data is still a relatively new finding and will require further investigation, the 1p19q implications have been well characterized and co-deletions of 1p19q, while not definitive for treatment modality, are prognostic which in turn might then affect the order of treatment. In general terms, if we have a low grade glioma patient that has a 1p19q deletion and we feel they need treatment, and surgery is not an option, we are more likely to treat with chemotherapy first and that treatment is usually Temozolomide. Having a low grade mixed glioma vs. a low grade astrocytoma increases the likelihood of 1p19q deletions
.
